| |
Bipolar disorder, also known as bipolar affective
disorder, manic-depressive disorder, or manic
depression, is a mental illness classified by
psychiatry as a mood disorder. Individuals with
bipolar disorder experience episodes of an elevated
or agitated mood known as mania alternating with
episodes of depression.
Those with bipolar disorder often describe their
experience as being on an emotional roller coaster.
Cycling up and down between strong emotions can keep
a person from having anything approaching a “normal”
life. The emotions, thoughts and behavior of a
person with bipolar disorder are often experienced
as beyond one’s control. Friends, co-workers and
family may sometimes intervene to try and help
protect their interests and health. This makes the
condition exhausting not only for the sufferer, but
for those in contact with her or him as well.
About 4% of people suffer from bipolar disorder.
Prevalence is similar in men and women and, broadly,
across different cultures and ethnic groups
In bipolar disorder, people experience abnormally
elevated (manic or hypomanic) mood states which
interfere with the functions of ordinary life. Many
people with bipolar disorder also experience periods
of depressed mood, but this is not universal. There
is no simple physiological test to confirm the
disorder. Diagnosing bipolar disorder is often
difficult, even for mental health professionals
Mania is the defining feature of bipolar disorder.
Mania is a distinct period of elevated or irritable
mood, which can take the form of euphoria, and lasts
for at least a week (less if hospitalization is
required). People with mania commonly experience an
increase in energy and a decreased need for sleep,
with many often getting as little as three or four
hours of sleep per night. Some can go days without
sleeping. A manic person may exhibit pressured
speech, with thoughts experienced as racing.
Attention span is low, and a person in a manic state
may be easily distracted. Judgment may be impaired,
and sufferers may go on spending sprees or engage in
risky behavior that is not normal for them. They may
indulge in substance abuse, particularly alcohol or
other depressants, cocaine or other stimulants, or
sleeping pills. Their behavior may become
aggressive, intolerant, or intrusive. They may feel
out of control or unstoppable, or as if they have
been "chosen" and are "on a special mission", or
have other grandiose or delusional ideas. Sexual
drive may increase. At more extreme levels, a person
in a manic state can experience psychosis or a break
with reality, where thinking is affected along with
mood. This can occasionally lead to violent
behaviors. The severity of manic symptoms can be
measured by rating scales such as the Altman
Self-Rating Mania Scale and clinician-based Young
Mania Rating Scale.
Hypomania is a mild to moderate level of elevated
mood, characterized by optimism, pressure of speech
and activity, and decreased need for sleep.
Generally, hypomania does not inhibit functioning as
mania does. Many people with hypomania are actually
more productive than usual, while manic individuals
have difficulty completing tasks due to a shortened
attention span. Some hypomanic people show increased
creativity, although others demonstrate poor
judgment and irritability. Many experience hyper
sexuality. Hypomanic people generally have increased
energy and increased activity levels. They do not,
however, have delusions or hallucinations.
Hypomania may feel good to the person who
experiences it. Thus, even when family and friends
recognize mood swings, the individual often will
deny that anything is wrong. What might be called a
"hypomanic event", if not accompanied by depressive
episodes, is often not deemed as problematic, unless
the mood changes are uncontrollable, volatile or
mercurial. If left untreated, an episode of
hypomania can last anywhere from a few days to
several years. Most commonly, symptoms continue for
a few weeks to a few months.
Signs and symptoms of the depressive phase of
bipolar disorder include persistent feelings of
sadness, anxiety, guilt, anger, isolation, or
hopelessness; disturbances in sleep and appetite;
fatigue and loss of interest in usually enjoyable
activities; problems concentrating; loneliness,
self-loathing, apathy or indifference;
depersonalization; loss of interest in sexual
activity; shyness or social anxiety; irritability,
chronic pain (with or without a known cause); lack
of motivation; and morbid suicidal thoughts. In
severe cases, the individual may become psychotic, a
condition also known as severe bipolar depression
with psychotic features. These symptoms include
delusions or, less commonly, hallucinations, usually
unpleasant. A major depressive episode persists for
at least two weeks, and may continue for over six
months if left untreated.
A mixed state, also known as dysphoric mania,
agitated depression, or a mixed episode, is a
condition during which features of mania and
depression, such as agitation, anxiety, fatigue,
guilt, impulsiveness, irritability, morbid or
suicidal ideation, panic, paranoia, pressured speech
and rage, occur simultaneously.
Typical examples include tearfulness during a manic
episode or racing thoughts during a depressive
episode. One may also feel incredibly frustrated or
be prone to fits of rage in this state, since one
may feel like a failure and at the same time have a
flight of ideas. Mixed states are often the most
problematic period of mood disorders, during which
susceptibility to substance abuse, panic disorder,
commission of violence, suicide attempts, and other
complications increase greatly.
A mixed state must meet the criteria for a major
depressive episode and a manic episode nearly every
day for at least one week. However, mixed episodes
rarely conform to these qualifications; they may be
described more practically as any combination of
depressive and manic symptoms.
Bipolar I disorder (pronounced "bipolar one" and
also known as manic-depressive disorder or manic
depression) is a form of mental illness. A person
affected by bipolar I disorder has had at least one
manic episode in his or her life.Most people are in
their teens or early 20s when symptoms of bipolar
disorder first appear. Nearly everyone with bipolar
I disorder develops it before age 50. People with an
immediate family member who has bipolar are at
higher risk.Many people with bipolar I disorder
experience long periods without symptoms in between
episodes. A minority has rapid-cycling symptoms of
mania and depression, in which they may have
distinct periods of mania or depression four or more
times within a year. People can also have mixed
episodes, in which manic and depressive symptoms
occur simultaneously, or may alternate from one pole
to the other within the same day.
A. Presence of only one Manic Episode and no past
Major Depressive Episodes.
Note: Recurrence is defined as either a change in
polarity from depression or an interval of at least
2 months without manic symptoms.
B. The Manic Episode is not better accounted for by
Schizoaffective Disorder and is not superimposed on
Schizophrenia, Schizophreniform Disorder, Delusional
Disorder, or Psychotic Disorder Not Otherwise
Specified.
DSM-IV- TRCriteria for Bipolar I Disorder, Most
Recent Episode Hypomanic
A. Currently (or most recently) in a Hypomanic
Episode.
B. There has previously been at least one Manic
Episode or Mixed Episode.
C. The mood symptoms cause clinically significant
distress or impairment in social, occupational, or
other important areas of functioning.
D. The mood episodes in Criteria A and B are not
better accounted for by Schizoaffective Disorder and
are not superimposed on Schizophrenia,
Schizophreniform Disorder, Delusional Disorder, or
Psychotic Disorder Not Otherwise Specified.
A. Currently (or most recently) in a Manic Episode.
B. There has previously been at least one Major
Depressive Episode, Manic Episode, or Mixed Episode.
C. The mood episodes in Criteria A and B are not
better accounted for by Schizoaffective Disorder and
are not superimposed on Schizophrenia,
Schizophreniform Disorder, Delusional Disorder, or
Psychotic Disorder Not Otherwise Specified.
DSM-IV-TRCriteria for Bipolar I Disorder, Most
Recent Episode Mixed
A. Currently (or most recently) in a Mixed Episode.
B. There has previously been at least one Major
Depressive Episode, Manic Episode, or Mixed Episode.
C. The mood episodes in Criteria A and B are not
better accounted for by Schizoaffective Disorder and
are not superimposed on Schizophrenia,
Schizophreniform Disorder, Delusional Disorder, or
Psychotic Disorder Not Otherwise Specified.
A. Currently (or most recently) in a Major
Depressive Episode.
B. There has previously been at least one Manic
Episode or Mixed Episode.
C. The mood episodes in Criteria A and B are not
better accounted for by Schizoaffective Disorder and
are not superimposed on Schizophrenia,
Schizophreniform Disorder, Delusional Disorder, or
Psychotic Disorder Not Otherwise Specified.
A. Criteria, except for duration, are currently (or
most recently) met for a Manic, a Hypomanic, a
Mixed, or a Major Depressive Episode.
B. There has previously been at least one Manic
Episode or Mixed Episode.
C. The mood symptoms cause clinically significant
distress or impairment in social, occupational, or
other important areas of functioning.
D. The mood episodes in Criteria A and B are not
better accounted for by Schizoaffective Disorder and
are not superimposed on Schizophrenia,
Schizophreniform Disorder, Delusional Disorder, or
Psychotic Disorder Not Otherwise Specified.
E. The mood symptoms in Criteria A and B are not due
to the direct physiological effects of a substance
(e.g., a drug of abuse, a medication, or other
treatment) or a general medical condition (e.g.,
hyperthyroidism).
Bipolar II disorder is a bipolar spectrum disorder
characterized by at least one episode of hypomania
and at least one episode of major depression.
Diagnosis for bipolar II disorder requires that the
individual must never have experienced a full manic
episode (one manic episode meets the criteria for
bipolar I disorder. The course of bipolar II
disorder is more chronic and consists of more
frequent cycling than the course of bipolar I
disorder. Bipolar II is associated with a greater
risk of suicidal thoughts and behaviors than bipolar
I or unipolar depression. Although bipolar II is
commonly perceived to be a milder form of Type I,
this is not the case. Types I and II present equally
severe burdens. Bipolar II is difficult to diagnose.
Patients usually seek help when they are in a
depressed state. Because the symptoms of hypomania
are often mistaken for high functioning behavior or
simply attributed to personality, patients are
typically not aware of their hippomanic symptoms.
As a result, they are unable to provide their doctor
with all the information needed for an accurate
assessment; these individuals are often misdiagnosed
with unipolar depression. Of all individuals
initially diagnosed with major depressive disorder,
between 40% and 50% will later be diagnosed with
either BP-I or BP-II. Despite the difficulties, it
is important that BP-II individuals are correctly
assessed so that they can receive the proper
treatment.
A. Presence (or history) of one or more Major
Depressive Episodes.
B. Presence (or history) of at least one Hypomanic
Episode.
C. There has never been a Manic Episode or a Mixed
Episode.
D. The mood symptoms cause clinically significant
distress or impairment in social, occupational, or
other important areas of functioning.
E. The mood episodes in Criteria A and B are not
better accounted for by Schizoaffective Disorder and
are not superimposed on Schizophrenia,
Schizophreniform Disorder, Delusional Disorder, or
Psychotic Disorder Not Otherwise Specified.
F. The symptoms cause clinically significant
distress or impairment in social, occupational, or
other important areas of functioning.
Cyclothymia or cyclothymic disorder is a relatively
mild mood disorder. In cyclothymic disorder, moods
swing between short periods of mild depression and
hypomania, an elevated mood. The low and high mood
swings never reach the severity of major depression
or mania.In cyclothymia, moods fluctuate from mild
depression to hypomania and back again. In most
people, the pattern is irregular and unpredictable.
Hypomania or depression can last for days or weeks.
In between up and down moods, a person might have
normal moods for more than a month -- or may cycle
continuously from hypomanic to depressed, with no
normal period in between.
A. For at least 2 years, the presence of numerous
periods with hypomanic symptoms (see p. 338) and
numerous periods with depressive symptoms that do
not meet criteria for a Major Depressive Episode.
Note: In children and adolescents, the duration must
be at least 1 year.
B. During the above 2-year period (1 year in
children and adolescents), the person has not been
without the symptoms in Criterion A for more than 2
months at a time.
C. No Major Depressive Episode, Manic Episode, or
Mixed Episode has been present during the first 2
years of the disturbance.
Note: After the initial 2 years (1 year in children
and adolescents) of Cyclothymic Disorder, there may
be superimposed Manic or Mixed Episodes (in which
case both Bipolar I Disorder and Cyclothymic
Disorder may be diagnosed) or Major Depressive
Episodes (in which case both Bipolar II Disorder and
Cyclothymic Disorder may be diagnosed).
D. The symptoms in Criterion A are not better
accounted for by Schizoaffective Disorder and are
not superimposed on Schizophrenia, Schizophreniform
Disorder, Delusional Disorder, or Psychotic Disorder
Not Otherwise Specified.
E. The symptoms are not due to the direct
physiological effects of a substance (e.g., a drug
of abuse, a medication) or a general medical
condition (e.g., hyperthyroidism).
F. The symptoms cause clinically significant
distress or impairment in social, occupational, or
other important areas of functioning.
The current thinking is that this is a predominantly
biological disorder that occurs in a specific part
of the brain and is due to a malfunction of the
neurotransmitters (chemical messengers in the
brain). As a biological disorder, it may lie dormant
and be activated spontaneously or it may be
triggered by stressors in life.
Although, no one is quite sure about the exact
causes of bipolar disorder, researchers have found
these important clues:
• Bipolar disorder tends to be familial, meaning
that it “runs in families.” About half the people
with bipolar disorder have a family member with a
mood disorder, such as depression.
• A person who has one parent with bipolar disorder
has a 15 to 25 percent chance of having the
condition.
• A person who has a non-identical twin with the
illness has a 25 percent chance of illness, the same
risk as if both parents have bipolar disorder.
• A person who has an identical twin (having exactly
the same genetic material) with bipolar disorder has
an even greater risk of developing the illness about
an eightfold greater risk than a nonidentical twin.
• Studies of adopted twins (where a child whose
biological parent had the illness is raised in an
adoptive family untouched by the illness) has helped
researchers learn more about the genetic causes vs.
environmental and life events causes.
Environmental Factors in Bipolar Disorder:
• A life event may trigger a mood episode in a
person with a genetic disposition for bipolar
disorder.
• Even without clear genetic factors, altered health
habits, alcohol or drug abuse or hormonal problems
can trigger an episode.
• Among those at risk for the illness, bipolar
disorder is appearing at increasingly early ages.
This apparent increase in earlier occurrences may be
due to underdiagnosis of the disorder in the past.
This change in the age of onset may be a result of
social and environmental factors that are not yet
understood.
Although the abnormalities in the brain due to
bipolar disorder are still unknown, the structural
abnormalities believed to be linked to bipolar
disorder are amygdala, basal ganglia, and the
prefrontal cortex. Research is currently being
conducted to find more definite information on the
definite causes and changes in the brain of bipolar
disorder.

Recently using MRI, hyperintense (bright white)
spots have been found in bipolar patients.
Hyperintensities have previously been associated
with a change in water content in the brain tissue,
but the causes of these are not known.
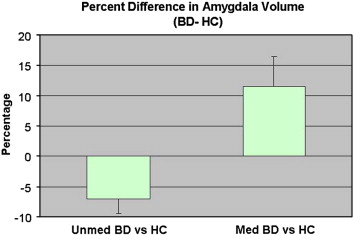
Amygdala volumes have been shown to be reduced in
unmediated patients and increased in medicated
patients. This is seen in the chart below.
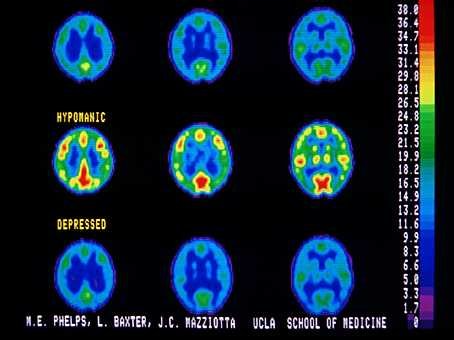
In this figure, normal brain scans are at the top,
hypomanic is in the middle row and depressed are at
the bottom. You can see the reduced activity in the
depressed brain, by the presence of more dark blue
and can see the over activity in the manic brain by
the presence of more green, yellow and red in the
brain scan.
BD patients and healthy control subjects
Abnormalities in the structure and/or function of
certain brain circuits could underlie bipolar.
Meta-analyses of structural MRI studies in bipolar
disorder report an increase in the volume of the
lateral ventricles, globuspallidus and increase in
the rates of deep white matter hyper intensities.
Functional MRI findings suggest that abnormal
modulation between ventral prefrontal and limbic
regions, especially the amygdale, likely contribute
to poor emotional regulation and mood symptoms.
Medication is a necessary part of treatment for
bipolar disorder but psychological treatment can
supplement medication.
Psychoeducational approaches typically help people
learn about the symptoms of the disorder, the
expected time course of symptoms, the biological and
psychological triggers for symptoms and treatment
strategies. Studies confirm that careful education
about bipolar disorder can help people adhere to
treatment with medications such as lithium.
Family focused treatment (FFT) aims to educate the
family about the illness, enhance family
communication and develop problem solving skills.
FFT leads to lower rates of relapse when added to
medication.
Lithium (brand names Eskalith, Lithobid) is the most
widely used and studied medication for treating
bipolar disorder. Lithium helps reduce the severity
and frequency of mania. It may also help relieve
bipolar depression.
Studies show that lithium can significantly reduce
suicide risk. Lithium also helps prevent future
manic and depressive episodes. As a result, it may
be prescribed for long periods of time (even between
episodes) as maintenance therapy.
Lithium acts on a person's central nervous system
(brain and spinal cord). It is thought to help
strengthen nerve cell connections in brain regions
that are involved in regulating mood, thinking and
behavior.
The dose of lithium varies among individuals and as
phases of their illness change. Although bipolar
disorder is often treated with more than one drug,
some people can control their condition with lithium
alone.
Benzodiazepines rapidly help control certain manic
symptoms in bipolar disorder until mood-stabilizing
drugs can take effect. They are usually taken for a
brief time, up to two weeks or so, with other
mood-stabilizing drugs. They may also help restore
normal sleep patterns in people with bipolar
disorder.
Benzodiazepines slow the activity of the brain. In
doing so, they can help treat mania, anxiety, panic
disorder, insomnia, and seizures.
Benzodiazepines prescribed for bipolar disorder
include (among others):
Ativan (lorazepam)
Klonopin (clonazepam)
Valium (diazepam)
Xanax (alprazolam)
Electroconvulsive therapy, also known as ECT or
electroshock therapy, is a short-term treatment for
severe manic or depressive episodes, particularly
when symptoms involve serious suicidal or psychotic
symptoms, or when medicines seem to be ineffective.
It can be effective in nearly 75% of patients.
For many individuals with bipolar disorder a good
prognosis results from good treatment, which, in
turn, results from an accurate diagnosis. Because
bipolar disorder can have a high rate of both
under-diagnosis and misdiagnosis, it is often
difficult for individuals with the condition to
receive timely and competent treatment.
Bipolar disorder can be a severely disabling medical
condition. However, many individuals with bipolar
disorder can live full and satisfying lives. Quite
often, medication is needed to enable this. Persons
with bipolar disorder may have periods of normal or
near normal functioning between episodes.
|
|

